By Dr. Richard C. Healy, ANJC Medicare Consultant
As Medicare Advantage plans gain popularity, many providers question the process of filing an appeal when they receive an organizational determination resulting in an adverse denial of a claim.
An Organizational determination is when an enrollee, or a provider acting on behalf of the enrollee, requests a pre-service organization determination if there is a question as to whether an item or service will be covered by the plan. If the plan denies an enrollee’s (or his/her treating provider’s) request for coverage as part of the organization determination process, the plan must provide the enrollee (and provider, as appropriate) with the standardized denial notice. These determinations or denials may be appealed.
Please use the following flow chart as a resource to file a Medicare Advantage Appeal:
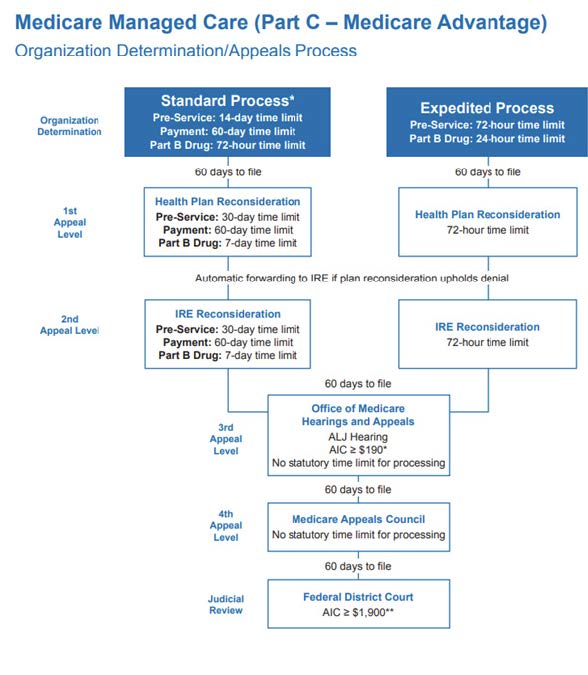
- AIC: Amount in Controversy
- ALJ: Administrative Law Judge
- IRE: Independent Review Entity
- *Plans must process 95% of all clean claims from out of
network providers within 30 days. All other claims must be
processed within 60 days. - **The AIC requirement for an ALJ hearing and Federal
District Court is adjusted annually in accordance with the
medical care component of the consumer price index.
The chart reflects the amounts for calendar year 2025.