Unravel the transformative evaluation and treatment techniques for SI joint dysfunctions and a nuanced understanding of pelvic mechanics. Gain insights on manipulation and muscle energy techniques from the in-depth perspective of Dr. Gregory H. Doerr, DC, CCSP, informed by over two decades of experience.
Chiropractors have been treating SI joint dysfunction for as long as we have been manipulating.
Is manipulation the only way to address these concerns? Are there times when manipulation is not the “answer” to an SI joint problem? Manipulation is obviously effective for SI disorders, but I discovered something 25 years ago that changed the way I treat some SI joint disorders.
I was working in a DC, PT, MD office when I was a student and during my first nine years in practice. During year one, the PT in our office came to me one day asking, “What was I doing differently than the other chiropractors?” I honestly could not figure out what I did differently. The PT further stated that when I manipulated the patients, they had less pain than when the other doctors did. I still had no answer. It took a few hours before I realized I did Pisiform pushes while the partners did more pull moves with the forearm laying across the SI joint.
Eric, the PT, and I spent some time discussing this issue and what we could do to further improve and isolate patients that had negative reactions.
The next few paragraphs will summarize the conclusions and treatments I have now used for over two decades.
The newest evaluation procedures I discovered have been well described and researched by people like Diane Lee and Andry Vleeming.
I was first exposed to some of these evaluations by Eric Brummer. The supine-to-sit test was completely new to me. At NYCC, I was taught deerfield testing. It never made much sense to me as it was too easy to influence, and only accessed from knee flexion while prone.
The supine-to-sit test to me was a wonderful assessment of pelvic mechanics…not that it did not have its faults. With the patient lying supine, the patient is asked to sit up. The clinician is to look at the ankles of the patient. I tend to rest my thumbs on the top of the medial malleolus. Then, the clinician looks for leg length changes from supine to sit. For the academic purpose of this article, we can state that while supine, the patient has a left short leg. Then, when the patient goes seated, the left leg appears to lengthen (or the right leg shortens, if you prefer).
Mechanically, this makes sense regarding pelvic mechanics and positioning.
Considering the situation above, if the left leg was short lying supine and it is not anatomical, and without fractures or surgery, we have to consider the pelvis.
It can be assumed that the left pelvis is in posterior rotation.
The simple reason for this is if the ilium is posterior, the acetabulum raises superiorly, creating a shorter limp while supine. However, when the patient goes to the seated position, the ilium rotates posteriorly. If the left ilium is already posterior (considering the minimal number of degrees at the SI joint), it can’t move much further posteriorly.
The compensation for a left posterior ilium is a right anterior ilium.
With the right side anterior, it has the ability to rotate further posteriorly, giving the appearance of the left leg lengthening as the acetabulum raises on the right side.
This test in itself is simply a screen.
The true test to ensure SI involvement are force closures at the SI joint.
Professor Vleeming described these force closures during a supine active straight leg raise. I prefer to perform these tests standing during LS ROM tests since the SI is really a weight-bearing joint. The key to performing these tests is to not compress the SI joint in a force closure parallel to the floor. Instead, the force closure should create vectors as if pushing to the top of a pyramid. One hand is placed on the PSIS pushing anterior and superiorly, and the other hand is placed on the ASIS pushing posterior and superiorly. The force closures are performed during painful LS ROM.
I frequently find extension and side flexion to be the most commonly involved with SI, but it can be any of the ranges. I ask the patient to rate their pain as a ten initially, then perform the painful ranges again while performing the force closures. If the pain reduces by at least 50% (rate a 5 or below), or the ROM increases drastically before pain starts, the SI joint is a primary cause of the pain.
It is important to remember that SI joint involvement history is frequently associated with pain in changes of position (sit to stand, in and out of a car, twisting in bed…and at times, hill or stair walking). It is also important to remember that SI pain can be local, L/S, or have radiation but not usually below the knee unless it is muscle referral patterns associated with the SI dysfunction.
Treatment for this disorder that we have found so effective for 25 years includes a combination of muscular and joint treatments.
MFR/IASTM to the pelvic stabilizers (glutes, piriformis), iliopsoas, TFL (especially with LE radiation), adductors, and the LS erectors and QL are the primary muscles I treat.
Interestingly enough, following just this treatment, you will find the LS ROM weight bearing has improved drastically without any joint treatment. Following the soft tissue treatment, I determine manipulation vs. muscle energy techniques for the joint issues. I tend to use manipulation more with men and muscle energy techniques with females who have had children in the past or currently pregnant. The pelvic angles as well as ligament stretching from hormones or past pregnancy, creates more of an imbalance in the pelvis in these patients.
I find muscle energy techniques to work extremely well in these situations without the risk of irritating the SI joint during manipulation. For muscle energy techniques for an L-PI, we will use the hip flexors (iliopsoas, rectus femoris, etc.) on the left side to “pull” the posterior side anteriorly and the hip extensors (glute max and hamstring) to “pull” the anterior pelvis posteriorly. This resets the pelvis into a normal position.
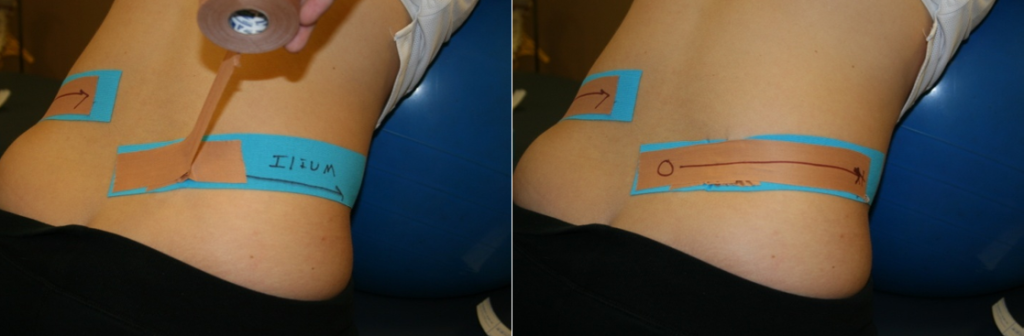
We can further stabilize this injury with exercises such as L-PI bridges (left leg straight and right leg bent bridges). Continued glute training and core training will continue to stabilize this injury. Also, the use of taping techniques for this condition will assist in stabilizing the patient when they have left the office.
R-PI Taping
R-PI Bridge Exercise

For references, please review the work of Diane Lee, The Pelvic Girdle (both texts), and Movement, Stability & Lumbopelvic Pain: Integration of Research and Therapy — 2nd Edition:
By Andry Vleeming PhD PT (Author), Vert Mooney MD (Author), Rob Stoeckart PhD (Author)
About the Author
Gregory H Doerr, DC, CCSP
Cliffside Park/Hackensack, NJ
functionalsofttissue.com
gdoerr@bergenchiropractic.com