By Gregory H Doerr, DC, CCSP
Rotator cuff impingement is one of the most common injuries chiropractors will see in their offices. Frequently, shoulder complaints make chiropractors nervous and are treated with the manipulation of the thoracic and cervical spine and A-P thrusts to the shoulder.
While manipulation to the Thoracic and Cervical spines can have important components to shoulder impingement, especially the Thoracic Spine associated with postural disorders, it is important to understand the common causes of shoulder impingement.
There are six common causes of subacromial shoulder impingement. Tensile Failure of rotator cuff fibers, poor scapular mechanics, rotator cuff imbalance, anterior capsular laxity, posterior capsule contracture, and supraspinatus outlet narrowing are the common reasons for this type of injury. Of these reasons for impingement, the one that is most commonly handled by chiropractors is poor scapular mechanics.
Scapular dyskinesis involves so many common situations that chiropractors deal with on a daily basis. Increased thoracic kyphosis, poor thoracic mobility, weakness in scapular stabilizers (especially lower and medial scapular stabilizers) create altered scapular mechanics leading to impingement. Maintenance of scapular dynamic stability with mobility of the glenohumeral joint keeps humeral head in constraint with glenoid throughout full range of motion of the shoulder. The scapula is protracted laterally and then anteriorly around the thoracic wall during throwing motions (arm acceleration and follow-through) which is controlled by eccentric contraction of medial and lower stabilizers. In abduction, the scapula moves laterally through first 30-50 degrees then rotates around a fixed axis until full elevation. Without this rotation acromion lift does not occur resulting in impingement.
In order to treat scapular dyskinesis, several treatment methods must be implemented:
- First manipulation of the thoracic spine and mobilization of the scapula are critical in assisting in restoring proper motion.
- Second, the muscles involved in scapular motion must be neurologically balanced. This can be accomplished by doing soft tissue treatments over the entire upper quadrant. The goal is to simply develop a hyperemia in the skin of the upper quadrant. Once a hyperemia has been created, the neurologic reset should have occurred.
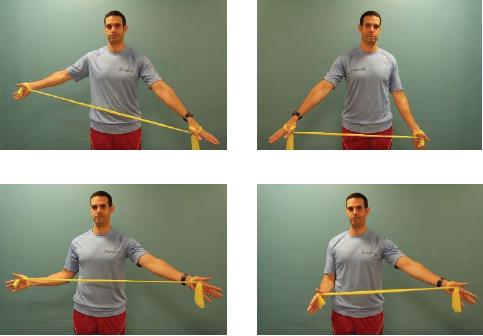
- Third, strengthening of the medial and lower scapular stabilizers as well as the serratus anterior are critical for long-term stabilization. Finally, we can use taping techniques for postural correction to assist the patient between treatments.

Rotator cuff imbalances are another reason for subacromial impingement. Imbalances in rotator cuff strength alter the dynamic stabilization of the glenohumeral joint. When we lose the balance in the rotator cuff, with rare exception, the ER of the shoulder become weaker than the IR, the head of the humerus is no longer balanced in the glenoid allowing for a narrowing of the subacromial space.
In order to treat this component of subacromial impingement, the doctor should focus on rebalancing the weakened rotator cuff with exercises.
Tensile failure of the rotator cuff involves a little more experience with shoulder injuries. Although rare, single-event traumas may cause rotator cuff injury. More commonly, repetitive micro-traumas are the cause. An example of this is the deceleration phase of overhead pitching. The eccentric contraction of the superior and posterior rotator cuff can result in tensile failure over continuous repetitive strain. Treatment of the rotator cuff includes a more aggressive soft tissue treatment to the involved tendons for the purpose of increasing fibroblastic activity and eccentric loading to increase collagen synthesis. Higher-pressure soft tissue treatments increase the number of fibroblasts in the tissue, and eccentric loading has been found to increase collagen synthesis in injured tendons drastically. By combining the two therapies, we can drastically increase the healing process of injured tendons. In the athletic situation, the doctor may also be involved in getting the patient to a coach that may properly restore or improve the athlete’s mechanics to help prevent future injuries.
The next reason for impingement is associated with the capsule of the shoulder.
Anterior laxity and posture capsule contracture can frequently present at the same time. Anterior laxity can easily be diagnosed using Relocation Test, and posterior capsule contracture can easily be discovered by watching for early and excessive anterior translation during supine passive IR.
When the shoulder translates anteriorly either due to laxity or being “pushed” forward from a posterior capsule contracture, it reduces the subacromial space creating impingement with overhead movements. Treatment of these conditions are slightly different. Posterior capsule contracture should be treated with soft tissue release of the posterior capsule and posterior glide mobilization to improve IR of the glenohumeral joint. Anterior laxity should be combated with both rotator cuff and scapular stabilization exercises.
Finally, AC outlet narrowing can cause impingement via 2 different possibilities. The AC outlet could be caused by either OA changes to the acromion or by congenital shape of the acromion. While it is not possible to change the shape of the acromion through conservative management, by improving posture, scapular mechanics, strengthening the scapular stabilizers and balancing the rotator cuff it may be possible to prevent more aggressive surgical intervention.

While the shoulder can be a daunting and complicated structure, following the above evaluation and treatment methods can quickly bring the shoulder into a more simplistic and manageable state. Having knowledge of soft tissue treatments, manipulation and mobilization, rehabilitation, and taping can make even the most complicated shoulder injury highly treatable.
References:
Willams GR, Martin K. Management of rotator cuff and impingement injuries in the athlete. Journal of Athletic Training. 2000; 35 (3): 300-315
Hovis WD, etal. Posterior instability of the shoulder with secondary impingement in elite golfers. Am J Sports Med. 2002 Nov/Dec; 30 (6): 886-890
Gehlsen, G. M., Ganion L. R., et al. (1999). Fibroblast responses to variation in soft tissue mobilization pressure.” Medicine & Science in Sports & Exercise, 31(4): 531-5
Langberg H, et al Eccentric rehabilitation exercise increases peritendinous type I collagen synthesis in humans with Achilles tendinosis. Scand J Med Sci Sports 2007;17:61-66.
Author Information:
Gregory H Doerr, DC, CCSP
Cliffside Park/Hackensack, NJ
functionalsofttissue.com
gdoerr@bergenchiropractic.com